FAQ
-
Remain completely hidden within the gums. If they aren’t able to emerge normally, wisdom teeth become trapped (impacted) within your jaw. Sometimes this can result in infection or can cause a cyst that can damage other teeth roots or bone support.
-
Emerge partially through the gums. Because this area is hard to see and clean, wisdom teeth that partially emerge create a passageway that can become a magnet for bacteria that cause gum disease and oral infection.
-
Crowd nearby teeth. If wisdom teeth don’t have enough room to come in properly, they may crowd or damage nearby teeth.
Impacted wisdom teeth can result in pain, damage to other teeth and other dental problems. In some cases, impacted wisdom teeth may cause no apparent or immediate problems. But because they’re hard to clean, they may be more vulnerable to tooth decay and gum disease than other teeth are.
Impacted wisdom teeth that cause pain or other dental complications are usually removed. Some dentists and oral surgeons also recommend removing impacted wisdom teeth that don’t cause symptoms to prevent future problems.
You can’t keep an impaction from occurring, but keeping regular six-month dental appointments for cleaning and checkups enables your dentist to monitor the growth and emergence of your wisdom teeth. Regularly updated dental X-rays may indicate impacted wisdom teeth before any symptoms develop.
According to the American Dental Association, wisdom teeth removal may be necessary if you experience changes in the area of those teeth, such as: pain, repeated infection of soft tissue behind the lower last tooth, fluid-filled sacs (cysts), tumors, damage to nearby teeth, gum disease, extensive tooth decay.
The decision to remove wisdom teeth isn’t always clear. Talk to your dentist or an oral surgeon about the position and health of your wisdom teeth and what’s best for your situation.
Impacted wisdom teeth can cause several problems in the mouth:
-
Damage to other teeth. If the wisdom tooth pushes against the second molar, it may damage the second molar or increase the risk of infection in that area. This pressure can also cause problems with crowding of the other teeth or require orthodontic treatment to straighten other teeth.
-
Cysts. The wisdom tooth develops in a sac within the jawbone. The sac can fill with fluid, forming a cyst that can damage the jawbone, teeth and nerves. Rarely, a tumor — usually noncancerous (benign) — develops. This complication may require removal of tissue and bone.
-
Decay. Partially impacted wisdom teeth appear to be at higher risk of tooth decay (caries) than other teeth. This probably occurs because wisdom teeth are harder to clean and because food and bacteria get easily trapped between the gum and a partially erupted tooth.
-
Gum disease. The difficulty cleaning impacted, partially erupted wisdom teeth increases the risk of developing a painful, inflammatory gum condition called pericoronitis in that area.
When a tooth is rocked back and forth during a traditional extraction, the force of the rocking damages the tissues in the tooth socket, which can cause pain for some time. Since atraumatic extraction is designed to minimize tissue damage, you’ll experience much less pain and bleeding after your tooth is removed, will recover faster and will have a lower risk of infection.
Tissue and small bits of the surrounding bone are often removed during a traditional extraction. With atraumatic tooth extraction, these structures remain undamaged. Atraumatic tooth extraction is often recommended if you plan to replace your tooth with a dental implant. Preserving as much bone as possible during the extraction provides a more stable foundation for your implant. If needed, bone grafts can be added to your jawbone immediately after an atraumatic extraction to build up the bone.
How dental implant surgery is performed depends on the type of implant and the condition of your jawbone. Dental implant surgery may involve several procedures. The major benefit of implants is solid support for your new teeth — a process that requires the bone to heal tightly around the implant. Because this bone healing requires time, the process can take many months.
-
lack of loading leads to gradual bone resorption
-
teeth shifting towards the gap
-
greater load on the remaining teeth causes inflammation of the tissues around and may lead to periodontitis
-
restoring teeth will be much harder, longer and more expensive over time
-
Damaged tooth removal
-
Jawbone preparation (grafting), when needed
-
Dental implant placement
-
Bone growth and healing
-
Abutment placement
-
Artificial tooth placement
The entire process can take many months from start to finish. Much of that time is devoted to healing and waiting for the growth of new bone in your jaw. Depending on your situation, the specific procedure done or the materials used, certain steps can sometimes be combined.
Once your gums heal, you’ll have more impressions made of your mouth and remaining teeth. These impressions are used to make the crown — your realistic-looking artificial tooth. The crown can’t be placed until your jawbone is strong enough to support use of the new tooth.
You and your dental specialist can choose artificial teeth that are removable, fixed or a combination of both:
-
Removable. This type is similar to a conventional removable denture and can be a partial or full denture. It contains artificial white teeth surrounded by pink plastic gum. It’s mounted on a metal frame that’s attached to the implant abutment, and it snaps securely into place. It can be easily removed for repair or daily cleaning.
-
Fixed. In this type, an artificial tooth is permanently screwed or cemented onto an individual implant abutment. You can’t remove the tooth for cleaning or during sleep. Most of the time, each crown is attached to its own dental implant. However, because implants are exceptionally strong, several teeth can be replaced by one implant if they’re bridged together.
-
Improved appearance
-
Improved speech. With poor-fitting dentures, the teeth can slip within your mouth, causing you to mumble or slur your words. Dental implants allow you to speak without the worry that teeth might slip
-
Improved comfort
-
Easier eating. Dental implants allow you to eat your favorite foods
-
Improved self-esteem
-
Improved oral health
-
Durability
-
Convenience. Dental implants eliminate the embarrassing inconvenience of removing dentures
When a tooth is lost the alveolar process begins to remodel. The vacant tooth socket collapses as it heals leaving an edentulous (toothless) area, termed a ridge. This collapse causes a loss in both height and width of the surrounding bone. In addition, when a maxillary molar or premolar is lost, the maxillary sinus pneumatizes in this region which further diminishes the thickness of the underlying bone. Overall, this leads to a loss in volume of bone that is available for implantation of dental implants, which rely on osseointegration (bone integration), to replace missing teeth. The goal of the sinus lift is to graft extra bone into the maxillary sinus, so more bone is available to support a dental implant.
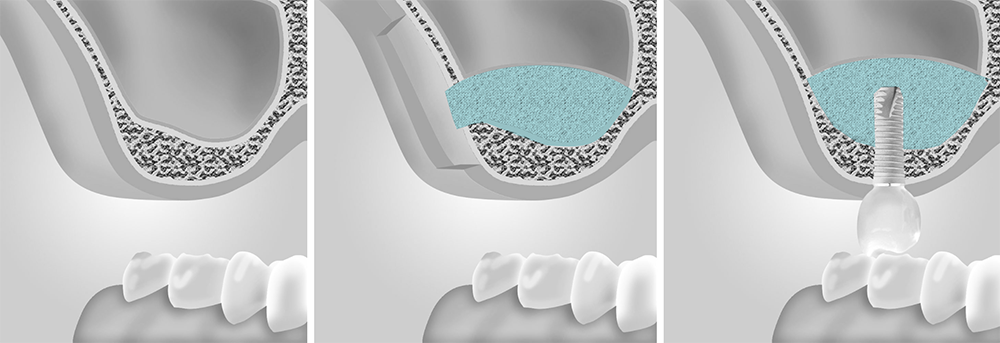
It takes about three to six months for the sinus augmentation bone to become part of the patient’s natural sinus floor bone.
For the next 4-6 weeks after the surgery you should avoid blowing your nose, sneezing through your nose, bending over: diving and flying by plane are prohibited for the next week after the surgery you should only be eating food that is soft, cool, and easy to chew. Do not eat anything spicy, hot, crunchy, tough to chew, or anything through a straw.
Using the lateral window technique (in what is called a “direct sinus lift”), the sinus membrane is lifted to make room for the required amount of bone, which is taken from another part of the patient’s body or from a cadaver.
During the procedure, the gum tissue is reflected to expose the jawbone, where a window is created into the sinus cavity. By pushing against this now-moveable piece of the jawbone (window) and moving it inward and upward into the sinus cavity, the sinus membrane is raised higher up. A bone graft is then placed into the now-empty space left behind by the raised membrane, and the area is stitched shut. Dental implants are placed 4 to 9 months later, which gives the bone graft time to mesh with the bone already there.
Osteotome Technique
The least invasive type of sinus lift incorporates the osteotome approach, in which elevating the sinus is immediately followed by the placement of the dental implant. The procedure begins with a small hole made in the jaw bone. Bone-grafting material is placed between the jaw bone and the sinus floor, increasing the space between them. The implant is then inserted. This technique is only appropriate in cases in which there is not enough bone to secure the implant, but enough bone to lend it some stability.
Your surgeon may talk to you about undergoing a bone graft for dental implants if he believes that your jaw bone is too thin or soft to keep the implant in place in its current state. If the bone cannot support the implant, it may cause the implant surgery to fail.
While autografts are often considered the “gold standard” because using a patient’s own bone makes the regeneration process more seamless, they aren’t possible in every case. Your dental professional will work with you to determine which bone graft procedure is right for you and will have the proper training to perform the surgery safely and effectively.
In 80-90 percent of cases I perform bone grafting and placing dental implant simultaneously
In 80-90 percent of cases I perform bone grafting and placing dental implant simultaneously.
The advantage of this approach is to save the patient’s time: bone grafting requires a long healing period (about 6 months). In case of simultaneous dental implantation and bone grafting, dental implant heals along with the bone. Thus, recovery from the surgery takes less time and, moreover, the patient DOES NOT REQUIRE a second surgery.
M. Nizhegorodskaya,
Ryazansky Avenue, 11, 205 office
Even numbers – morning (8:00-14:00)
Odd numbers – evening (14:00-20:00)
Lev Yashin Street 7, ALVI DENT
Contact us
M. Nizhegorodskaya,
Ryazansky Avenue, 11,
205 office
Even numbers – morning (8:00-14:00)
Odd numbers – evening (14:00-20:00)
Lev Yashin Street 7, ALVI DENT
Contact us